Together against pneumococcal diseases.
The pneumococcal diseases group a certain type of infections caused by a bacteria called Streptococcus pneumoniae. These diseases can range from ear and sinus infections to pneumonia and bloodstream infections.1
Yearly, Streptococcus pneumoniae causes nearly 5800 hospitalisations2 and 430 deaths2 in Belgian adults above the age of 50. For the 65+ population, the mortality rate reaches 12%.3
430 patients above the age of 50 die of IPD* every year.2
On a yearly basis, Invasive Pneumococcal Diseases result in death for 430 Belgian adults above the age of 50.2
This is roughly the amount of people you would need to fill 3 busses.
Yearly, 5800 patients above the age of 50 get hospitalised.2
5800 Belgian patients end up in the hospital because of a pneumococcal infection.2 These patients are all adults above the age of 50.
This is almost 6 times the entire population of Flanders’ smallest city.4
The Superior Health Council recommends vaccination3 for IPD.*
The Superior Health Council has been recommending pneumococcal vaccination for healthy adults above the age of 653, and certain groups at risk since 2014.
WHY is there no publicly funded program in place?

Why is there no publicly funded program for adults in place?
Despite a positive recommendation from the Belgian Superior Health Council, the vaccination rate in Flanders is very low (only 8.6%5), much lower than influenza (51.9%5) and COVID-19 (80%).6 This is partly due to the fact that the vaccine is not publicly funded for adults in Belgium.
There is a momentum of European countries like the Netherlands, Denmark and Sweden who already have a government funded program.7, 8, 9
Belgium is one of the only Western European countries without a publicly funded program for adults.7–15
What are the numbers on
hospitalisation and deaths?
For adults above the age of 50, the chance at hospitalisation is lower in comparison to adults above the age of 65. Yet, pneumococcal diseases cause 5800 adults above the age of 50 to be hospitalised every year.2
As people get older, the chance of developing severe symptoms leading to hospitalisation and death increases. For adults above the age of 65, the mortality rate is 12%. For adults above the age of 85, the percentage doubles to a mortality rate of 24%.3
How can we prevent pneumococcal diseases
Several ways of protection against pneumococcal diseases exist, with appropriate hygienic measures and with vaccination.
You need to avoid any close contact with sick people. You need to wash your hands regularly and to adopt hygienic measures when you sneeze, cough or blow your nose.
You can also get vaccinated.
Is vaccination recommended?
Due to the high number of yearly hospitalisations and deaths, and the great risk at cardiovascular complications, vaccination is recommended by both health officials and the Superior Health Council.3
Despite this recommendation, less than 10% of the adults at risk get vaccinated.3 There is also no publicly funded vaccination program in place.
Why is there no vaccination program in place?
The low vaccination rate is is partly due to the lack of publicly funded vaccinations for adults. In contrast to other Western European countries, like The Netherlands, Denmark and Sweden, Belgium does not have publicly funded vaccinations for adults.7, 8, 9 Therefore we must raise awareness to the severity of this disease and the need for a publicly funded vaccination for older adults.

This is how you can help!
You can help by raising awareness if you agree that pneumococcal diseases can have an important impact and that preventive measures are needed.
You can do this by sharing this webpage, talking to your friends and family, or by downloading and sharing the information brochure on pneumococcal diseases and their consequences.
For more info on pneumococcal diseases, visit www.pneumoinfo.be
* IPD: Invasive Pneumococcal Diseases
* SHC: Superior Health Council
References
1. https://www.gezondheidenwetenschap.be/richtlijnen/preventie-van-ernstige-pneumokokkeninfecties. Last Access: 01/2023.
2. Federaal Kenniscentrum voor Gezondheidszorg. Welke Pneumokokkenvaccinatie bij ouderen? KCE; 2016 Rapport 274As. Last Access: 01/2023.
3. Hoge Gezondheidsraad. Vaccinatie tegen pneumokokken (volwassenen). Brussel: HGR; 2022. Advies nr 9674. Last Access: 01/2023.
4. https://nl.wikipedia.org/wiki/Lijst_van_steden_in_Vlaanderen. Last Access: 01/2023.
5. https://www.sciensano.be/sites/default/files/va_nl_2018.pdf. Last Access: 01/2023.
6. https://covid-vaccinatie.be/en. Last Access: 01/2023.
7. https://www.nivel.nl/sites/default/files/bestanden/1004078.pdf. Last Access: 01/2023.
8. https://www.ssi.dk/aktuelt/nyhedsbreve/epi-nyt/2020/uge-44-45—2020. Last Access: 01/2023.
9. https://www.folkhalsomyndigheten.se/the-public-health-agency-of-sweden/communicable-disease-control/vaccinations/vaccination-programmes/#:~:text=In%20Sweden%2C%20children%20are%20offered,children%20and%20adults%20at%20risk. Last Access: 01/2023.
10. https://www.hse.ie/eng/health/immunisation/hcpinfo/othervaccines/pneumo/. Last access: 01/2023.
11. https://www.gov.uk/government/publications/vaccine-update-issue-320-april-2021-european-immunisation-week-special-edition/vaccine-update-issue-320-april-2021-european-immunisation-week-special-edition. Last access: 01/2023.
12. https://www.sanidad.gob.es/en/profesionales/saludPublica/prevPromocion/vacunaciones/programasDeVacunacion/docs/Neumococo_Gruposriesgo.pdf. Last access: 01/2023.
13. https://www.dgs.pt/normas-orientacoes-e-informacoes/normas-e-circulares-normativas/norma-n-0112015-de-23062015-pdf.aspx. Last access: 01/2023.
14. https://www.ordinefarmacistirimini.it/files/indicazioni_organizzative_per_lofferta_ai_65enni_della_vaccinazione_antipneumococcica.pdf. Last access: 01/2023.
15. https://szu.cz/tema/vakciny/ockovaci-kalendar-v-cr?highlightWords=O%C4%8Dkovac%C3%AD+kalend%C3%A1%C5%99+%C4%8CR. Last access: 01/2023.
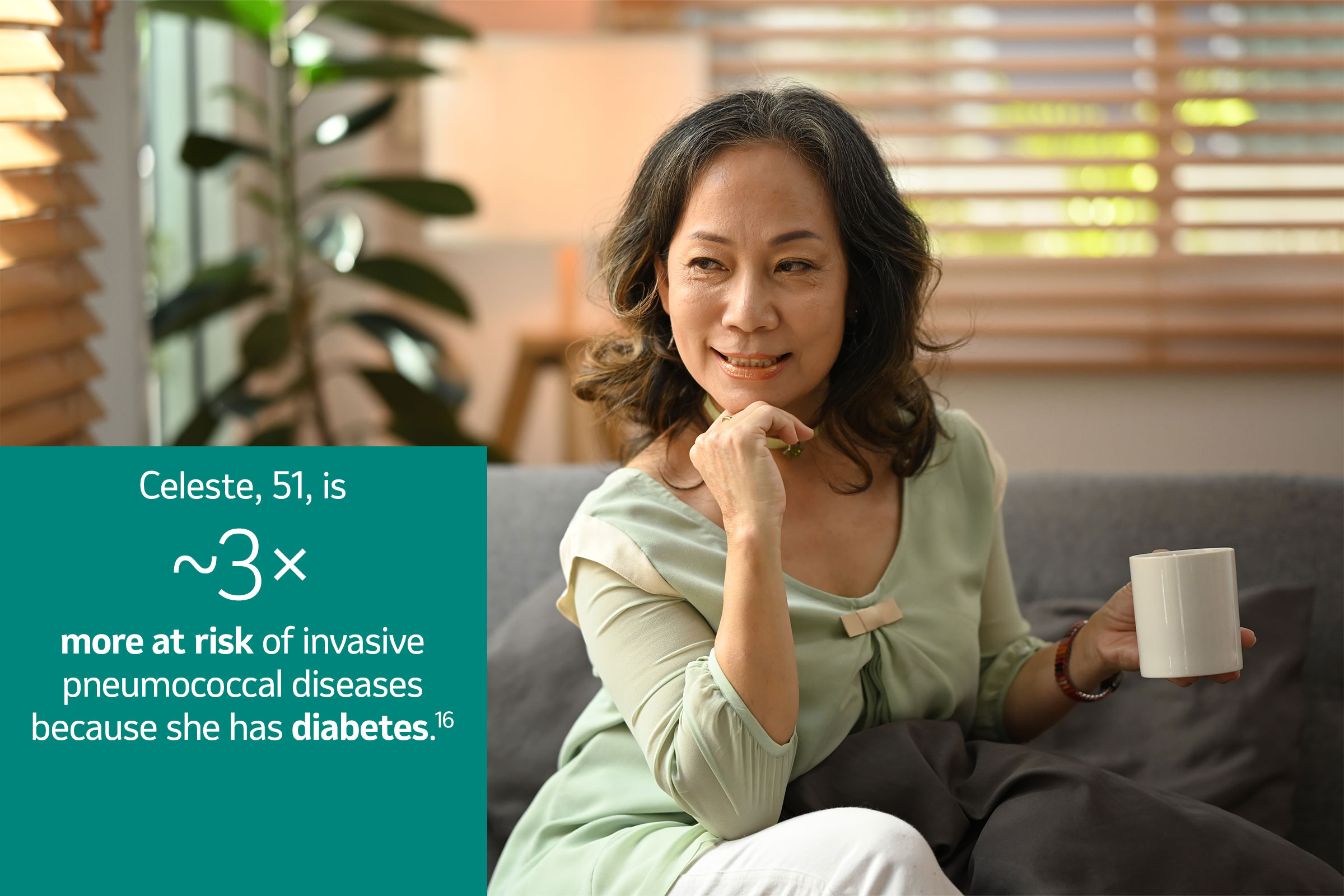
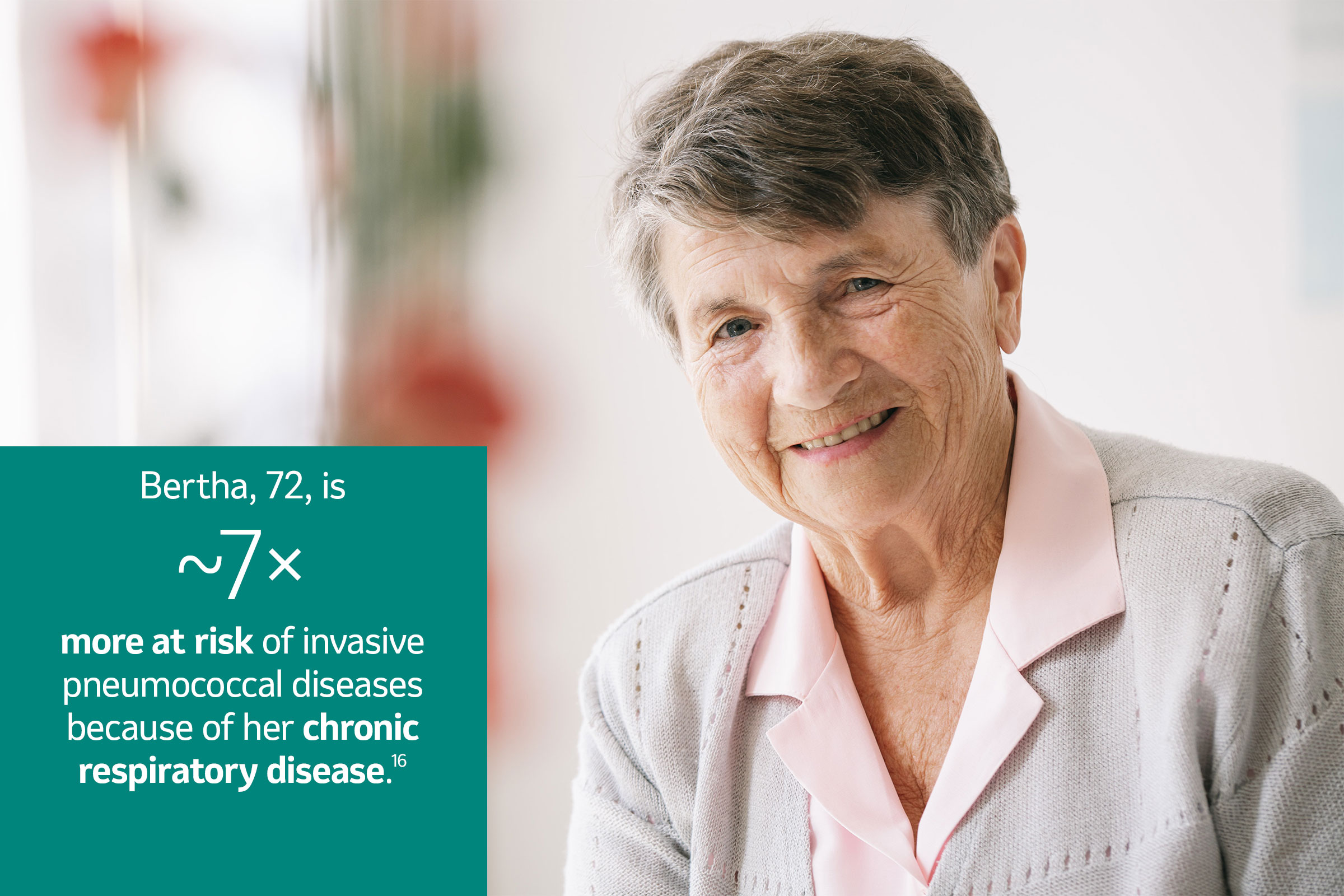
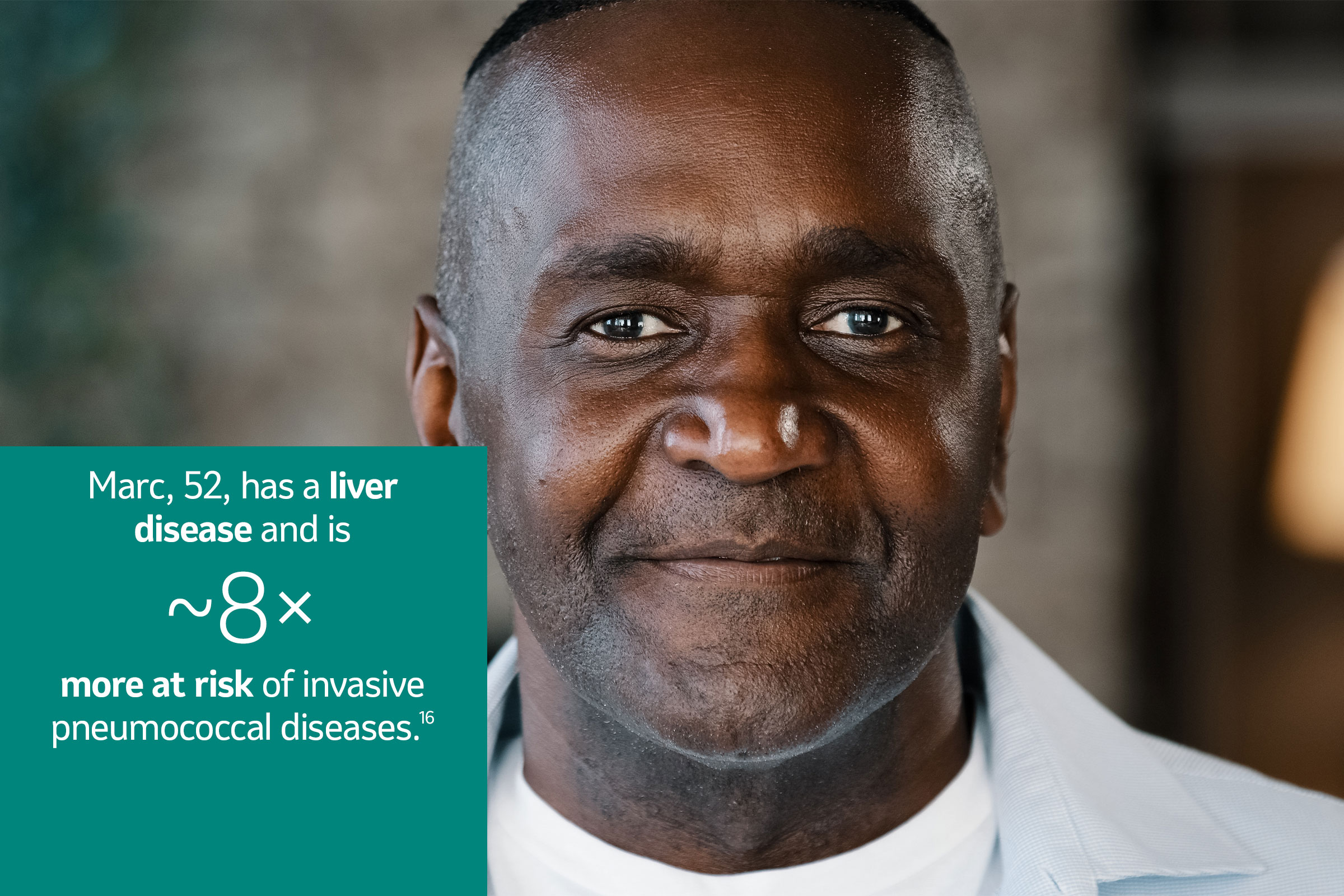
16. Kimberly M. et al. Rates of pneumococcal disease in adults with chronic medical conditions. Pneumococcal disease in adults OFID 2018.
BE-NON-01594. Date of last revision: 03/2023.